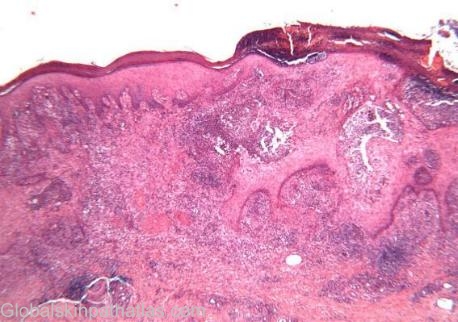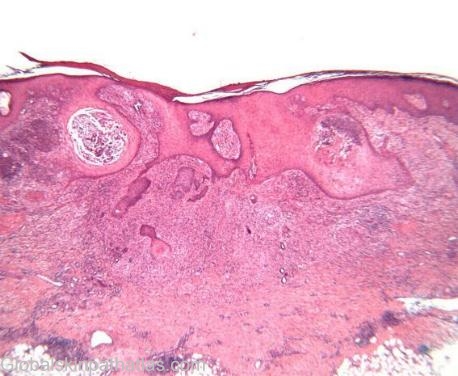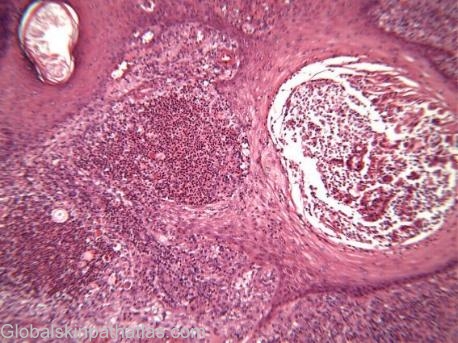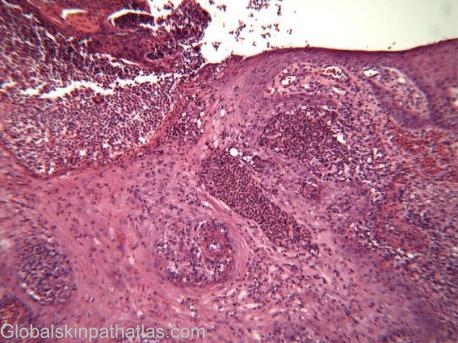
Diagnosis: Sporotrichosis
Description:
Clinical Features: Nodule
Pathology/Site Features: Granulomas
Sex: M
Age: 45
Submitted By:
Differential DiagnosisHistory:
Case submitted by Dr Adrian Cachia Dermatopathologist
A 53 year old otherwise healthy man presented with a 3 month history of a solitary plaque on the dorsum of his right hand. A biopsy was taken
Sporothrix schenckii lives as a saprophyte on plants in many areas of the world (including Australia, especially in tropical and subtropical regions). In nature and on culture at room temperature the fungus grows as a mould, but within host tissue or at 370C on enriched media it grows as a budding yeast. Identification is by the appearance of the fungus in mould and yeast forms. Small spores with hairlike attachment to hyphae give the fungus the name Sporothrix.
Pathogenesis and pathology:
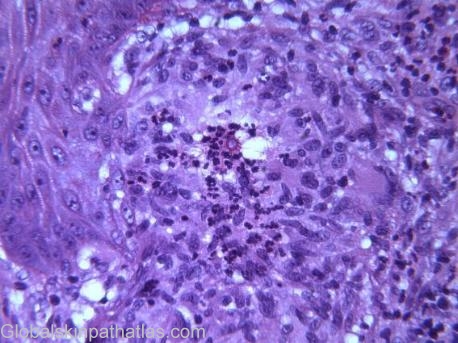
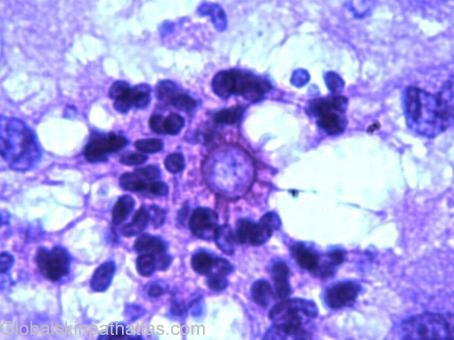
Infection results when minor trauma inoculates the fungus into subcutaneous tissue. Nursery workers, florists, and gardeners acquire the illness from roses, sphagnum moss, and other plants. Infection may be limited to the site of inoculation (plaque sporotrichosis) or extend along proximal lymphatic channels (lymphangitic sporotrichosis). Spread on an extremity, the usual site, even as far as an inguinal or axillary node is rare and hematogenous dissemination from the skin remains unproven. The portal for osteoarticular, pulmonary, and other extracutaneous forms of sporotrichosis is unknown but is likely the lung. Untreated sporotrichosis shows little evidence of self-healing and is capable of extreme chronicity. The inflammatory response contains both clusters of neutrophils and a marked granulomatous response with epithelioid cells and giant cells. There is often a blastomycosis-like pseudoepitheliomatous hyperplasia of the epidermis, with claw-like extensions of epidermis extending into the dermal granulation tissue, and with partial transepidermal elimination of the infected material. The diagnosis is made by finding the fungus with a classical stellate appearance known as a ‘sporotrichoid body’ in the tissue sections, or by fungal culture or PCR.
Clinical manifestations:
Lymphangitic sporotrichosis forms a nearly painless red papule at the site of inoculation. Over the next several weeks, similar nodules form along proximal lymphatic channels. Nodules intermittently discharge small amounts of pus. Ulceration may occur. The proximal extension of these lesions, often with skip areas, is quite distinctive, but may be mimicked by lesions of Nocardia brasiliensis. Mycobacterium marinum. or, on rare occasions, by Leishmania brasiliensis or M. kansasii.
Plaque sporotrichosis is a nontender red maculopapular granuloma confined to the site of inoculation. Osteoarticular sporotrichosis presents as mono- or polyarticular arthritis of indolent onset and progression over months or years, involving the elbows, knees, wrists, ankles, and, rarely, smaller joints of the extremities. Periarticular bone gradually appears "moth-eaten," and draining sinuses may appear over joints and bursas. Hematogenous spread to the skin may be observed during polyarticular disease, but none of the skin lesions show lymphangitic spread. Immunosuppression predisposes to such spread. Pulmonary sporotrichosis usually presents as a single chronic cavitary upper-lobe lung lesion.
Diagnosis:
Culture of pus, joint fluid, sputum, or skin biopsy specimen is the preferred method of diagnosis. The appearance of S. schenckii in tissue is quite variable. In skin lesions, organisms are hard to find.
Treatment:
Cutaneous sporotrichosis can be cured with oral administration of a saturated solution of potassium iodide, given in increasing divided daily doses up to 4.5 to 9 mL per day for adults, as tolerated. Gastrointestinal disturbance or acneform rash over the cape area and face are common, but therapy should be continued for 1 month after resolution of all lesions. Patients with serious allergic reactions to iodides may respond to local heat, particularly when plaque sporotrichosis is the only form of disease. Extracutaneous sporotrichosis rarely responds to iodides, but cures have been obtained in over half such patients with prolonged courses of intravenous amphotericin B.